March 9, 2020
This morning, the U.S. Department of Health and Human Services Secretary Alex Azar, National Coordinator of Health IT Don Rucker, Centers for Medicare and Medicaid Services Administrator Seema Verma, and Matthew Lira from the White House Office of American Innovation jointly announced the long-awaited final rules on information-blocking and interoperability, part of a national strategy to transform medicine into a data-driven enterprise. The new rule from the Office of the National Coordinator for Health Information Technology (ONC) promotes nationwide secure, standardized, and interoperable health information technology, as called for under the 21st Century Cures Act.
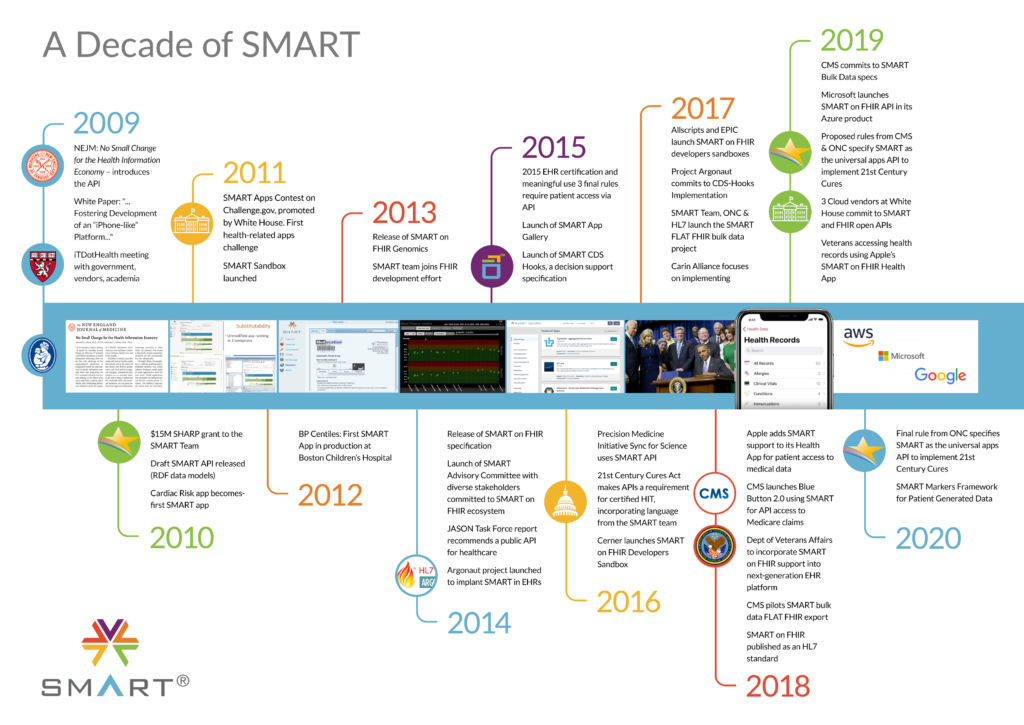
Over a decade has passed since the 2009 New England Journal of Medicine article, in which researchers at the Boston Children’s Hospital Computational Health Informatics Program introduced the idea of an application programming interface (API) to promote an apps-based health information economy and an “app store” model for health.
The ONC granted funds for the development of the SMART on FHIR API in 2010. Now, ten years later, the SMART on FHIR API is universally required so that an app written once can run anywhere in the healthcare system, and gain access to all of the elements of a patient’s electronic data, without special effort.
The Final Rule from the ONC supports seamless and secure access, exchange, and use of electronic health information, requiring standardized APIs to enable patients to securely access computable copies of their health records via smartphones.
The Final Rule also requires, for certified HIT, SMART/HL7 Bulk Data Export/Flat FHIR API, which will enable ready and secure access to population level data sets from electronic health records. Boston Children’s Hospital worked with HL7 to enable push-button population health, which should make it turnkey to extract data from EHR systems. Streamlined aggregation and analysis of data at a population level will lead to improved population health management, value-based care delivery, and opportunities for discovery science.
You must be logged in to post a comment.